Prediabetes And The Sugar Crash Roller Coaster
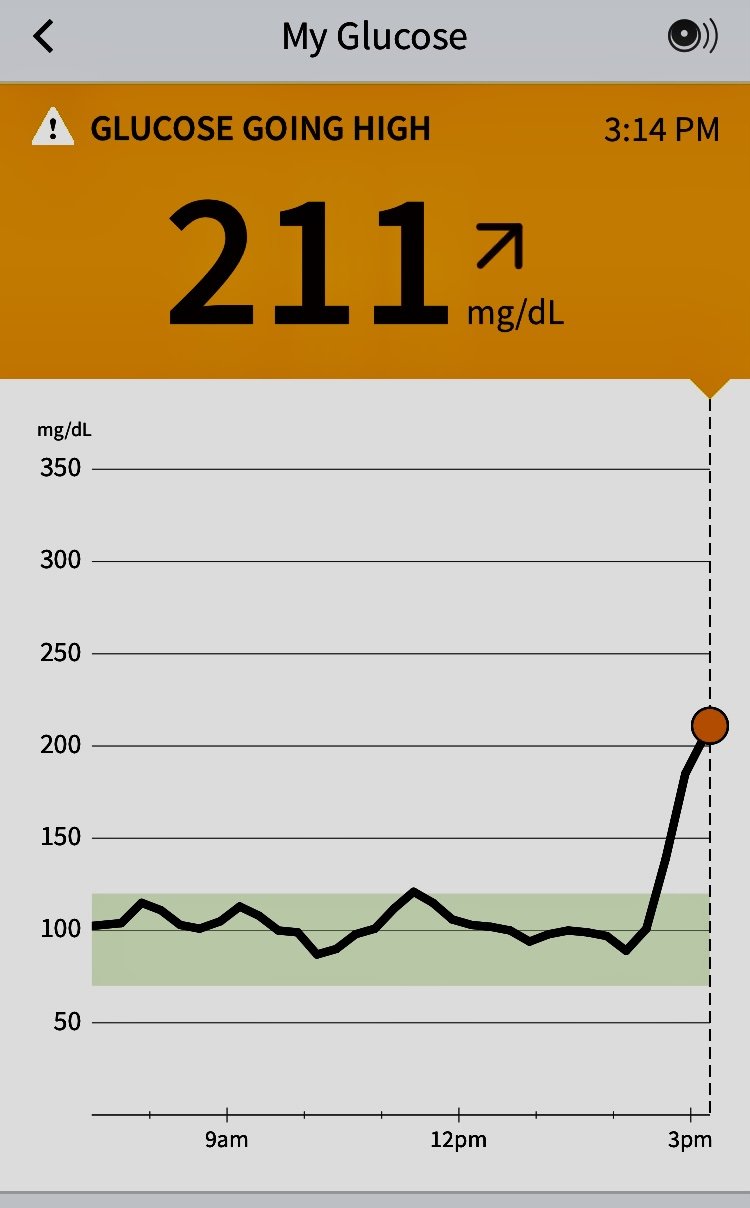
This is my own blood sugar after eating pasta. I wear a continuous glucose monitor to keep me honest about how my food choices affect my metabolism.
A 6 minute read
Have you been told by your doctor that you have pre-diabetes? Are you worried about your blood sugar levels and your family history of prediabetes and diabetes? If so, you are not alone. The CDC estimates that 1 in 10 Americans currently have diabetes. Even more shocking are the statistics for prediabetes, which is estimated to affect 1 in 3 people, many who are unaware they have prediabetes. Prediabetes puts you at a high risk of developing diabetes (as well as heart disease and stroke). Read the full CDC National Diabetes Statistics Report, 2020 here.
If you have a glycosylated hemoglobin level (A1C) of 5.7% to 6.4% you fall in the prediabetes category of this disease. Have an A1C level of 6.5% or higher and your doctor has probably diagnosed you with diabetes.
If you don’t know your A1C (glycosylated hemoglobin or HbA1C) level, talk with your doctor about getting this lab test included with your annual blood work. A1C is an average of your blood sugar levels over the last 3 months. It is a much better screening tool than the fasting glucose you see on your annual blood work. The higher your A1C, the higher your average daily blood sugar has been. For example, if you have and A1C of 5.9%, you know that your averaged daily blood sugar is 123. You can see a chart of A1C levels and how they correlate to average daily blood sugar here. A good goal is to aim for an average daily blood sugar of 99 which correlates to an A1C of about 5.1.
Lifestyle factors such as diet and exercise play a big role in helping to bring balance back to your blood sugar levels. Prevention is key, and living a preventive lifestyle is perhaps the single most important action we can all take to help reduce the risk of type 2 diabetes and prediabetes.
What is the Difference Between Type 1 and 2 Diabetes?
Type 1 Diabetes
Previously known as insulin-dependent or juvenile diabetes, Type 1 Diabetes is an auto-immune condition in which the body’s immune system attacks the pancreas, killing the insulin producing beta islet cells, preventing them from producing enough insulin. Close monitoring and lifelong insulin therapy are necessary. Type 1 diabetes care is highly specialized and is beyond the scope of this blog and my practice.
Type 2 Diabetes
Type 2, aka adult onset, or non-insulin-dependent diabetes can develop after years of imbalanced blood sugar levels cause the body to develop a resistance to insulin. When the cells stop responding to insulin, they can’t easily take up glucose from your blood, leading to higher-than-normal blood sugar levels.
Type 2 diabetes and prediabetes become more common as we get older and is particularly prevalent after 45 years of age. Sadly, we are now seeing type 2 diabetes in more younger people than ever before. By the time pre diabetes is discovered, metabolic intolerance has been going on for years.
The Blood Sugar Roller Coaster
Blood glucose highs and lows aren’t only for people with diabetes and prediabetes. In fact, it is normal for our glucose levels to fluctuate throughout the day as we eat. Our body tightly regulates our blood sugar levels by storing the glucose in our cells to be used as energy.
When we eat a healthy, whole foods diet that is low in sugar and contains plenty of fiber, it is relatively easy to stay satiated and resist temptation. But once we start to rely on sugar and coffee to make it through the afternoon, we quickly run into problems.
If you are someone who gets “hangry”, the following description of Reactive Hypoglycemia won’t come as a surprise:
Reactive Hypoglycemia…No Way to Live
1 - A high sugar snack is eaten (candy bar, pastry, sweet cereal etc.)
2 - Blood sugar levels rise fast, causing the pancreas to send out an emergency flood of insulin to move that glucose out of the blood and into the muscles.
3 - Blood glucose drops fast due to the flood of insulin, making you feel hungry again, with a particular craving for a sweet treat.
4 - You reach for another high sugar snack to feed the craving, inadvertently starting the roller coaster ride all over again.
Some common symptoms that are often blamed on stress or aging may in fact be due to long term issues with high blood sugar and prediabetes. These include:
Mood Swings
Do you regularly “crash” after a carbohydrate-heavy meal or sweet snack? Do you feel shaky, irritable, and “hangry” when you haven’t eaten in a while? Mood swings, including bursts of energy followed by rapidly depleted energy, are often in response to wide fluctuations in blood sugar.
Sugar Cravings
Another frustrating irony is that high blood sugar leads to cravings for more carb-heavy and sugary foods, further adding to the cycle of insulin resistance. I tell clients all the time that the more sugar and carbohydrate you eat the more you want. It really is a vicious cycle.
An “Abdominal Apron” of Belly Fat
When your body senses high glucose levels, it secretes more insulin to trigger your cells to absorb the excess glucose. However, insulin (an anabolic hormone) also encourages fat storage AND discourages fat release, especially around the belly. A blood sugar spike = high blood sugar = high insulin (anabolic hormone) = fat storage and weight loss resistance.
Hormone Imbalance
Healthy female hormones and blood sugar are intricately interconnected. Excess insulin causes the body to produce increased amounts of testosterone, and belly fat tissue converts this excess testosterone into estrogen. This scenario can lead to an imbalance between estrogen and progesterone that can bring on symptoms such as anxiety, depression, insomnia, fertility issues, and more.
Lifestyle Factors to Help Support Your Blood Sugar Levels
As mentioned, blood sugar highs and lows and the risk of type 2 diabetes are very much related to lifestyle, and certain lifestyle choices can greatly impact how well your body manages blood glucose. Here are my top tips for preventing prediabetes from advancing to diabetes:
Know your numbers
This is hands down the best way to get diabetes and prediabetes under control. Continuous glucose monitors like the Free Style Libre are a simple way to know how your blood sugar responds to meals, activity, medications, and stress at a single moment in time, as well as over the course of a day or week.
I find that once my clients start wearing a sensor, while working closely with me, they make huge progress in controlling their blood sugars and losing weight. Clients who wear a CGM love the immediate feedback on food choices and how it positively influences what and when they eat.
You do not need to wait for a diagnosis of diabetes before you continuously monitor your blood sugar. Interested in how I work with clients to control diabetes and pre-diabetes? Click here to book a call.
More Fiber
With its many health benefits for the gut, digestion and alleviating constipation, fiber intake has been linked to increased insulin sensitivity and lower blood sugars. Including foods with a high fiber content in all meals can help to reduce how high blood sugar spikes. I am talking about (organic) vegetables here. Aim for a big bowl of lightly steamed vegetables at every meal. Avoid the starchy type of vegetables (potatoes and corn). Limit fruit to organic berries once each day. Fruit is not your friend when you are trying to get blood sugar under control. Whatever you do, avoid juice. See my blog on fiber here.
Leafy Greens
Spinach, kale, broccoli, and cauliflower have been researched for their role in helping reduce the risk of type 2 diabetes, likely because of their fiber and high concentrations of minerals as well as antioxidant polyphenols and vitamin C. Aim for at least 2 servings each day.
Low Glycemic Foods
The glycemic index was developed to measure a food’s impact on blood sugar. The higher the food is found on the index the faster it spikes blood sugar, while the foods found on the lower end of the glycemic index are more slowly digested and absorbed. Note that the glycemic index only applies to foods that contain carbohydrates. Several studies have found that following a low glycemic diet can reduce the risk of developing type 2 diabetes and prediabetes.
Following a low glycemic diet doesn't have to be difficult, and lists are readily found on Google. Try swapping high-GI white bread for a lower-GI choice like 100% rye bread. I have found that this useful index is, does not give you the personal, actionable, information that wearing a continuous glucose monitor does
Drinks Matter
Sweet beverages can contain a surprising amount of sugar, and one study found that people who drank at least one sweet drink a day had a 26 percent higher chance of developing diabetes!
I hope it goes without saying that sodas have no place in the diet of anyone struggling with prediabetes and diabetes.
Juice
Fruits are naturally high in sugar, and by juicing them you may find yourself knocking back multiple servings in one go, guaranteeing a sugar spike (that’s even the case when it comes to unsweetened fruit juice). People who wear a CGM find that juice of any kind raises their blood sugar just like a regular soda does. It is best to avoid all juice if you a re trying to control diabetes or prediabetes.
Smoothies
Blending fruit into a smoothie means you keep the fiber, which is good, however it is easy to overdo the sugar content. Try reducing the sweet ingredients (i.e., limit yourself to a few berries) and give alternatives such as avocado and nut butters a try. These higher fat ingredients help to increase satiety, so a smaller smoothie is often enough.
Water
When it comes to managing blood sugar, let’s not forget about the importance of fresh, filtered water. Avoid water in plastic bottles if possible (contains nasty chemicals). It helps you to stay hydrated, keeps your digestion moving and your cells healthy, and is vital for inter-cellular communication.
Get a Good Night’s Sleep
High blood glucose levels can seriously impair your ability to get a good night’s sleep and a poor night’s sleep can adversely affect your blood sugar. Make good sleep a priority by practicing good sleep hygiene, including turning off all devices an hour before bed, sleeping in a cool, dark room and limiting drinks of any kind before bedtime.
Become Purposeful About Exercise
Exercise helps maintain healthy blood sugar levels by increasing insulin sensitivity and making your muscles more efficient at glucose absorption. Studies suggest high-intensity interval training is the most effective at burning sugar, but any form of cardio that you can maintain over the long haul, along with some resistance training, is an excellent and sustainable approach. Yoga and Pilates have a good mix of strength, cardio and relaxation and have been researched for their positive impact on stabilizing blood sugar in diabetes patients.
Taking a walk around the block after dinner each night is an excellent habit which allows your body to burn off some glucose so that you sleep better - and as controversial as it may be in some families, being the one who does the dishes and tidies up before bed can be just as effective.
Supplements
The judicious use of supplements can be an important addition to a healthy diet and lifestyle for someone working to reverse diabetes and prediabetes. A thorough assessment of vitamin and mineral adequacy is part of my work up with all clients. There are many nutrient inadequacies that can interfere with the reversal of diabetes and prediabetes. Almost all minerals influence the transport of sugar into the cell. Vitamin D is a huge player in blood sugar metabolism as well and there are many herbs and bioactives that can be useful in normalizing blood sugar. I recommend pharmaceutical grade supplements and I make no profit on the supplements I recommend.
In Summary…
The complications that arise when we don’t properly manage our blood glucose over time are serious. They can include heart, blood vessel and nerve damage, kidney disease, and eye damage. However, taking charge of the necessary lifestyle factors can give great results in a short amount of time.
If you are ready to understand your blood sugar levels and reverse diabetes or prediabetes, give me a call.
Sources
Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2020
Stanhope KL. Sugar consumption, metabolic disease and obesity: The state of the controversy. Crit Rev Clin Lab Sci. 2016;53(1):52-67. doi: 10.3109/10408363.2015.1084990. Epub 2015 Sep 17. PMID: 26376619; PMCID: PMC4822166.
Adams OP. The impact of brief high-intensity exercise on blood glucose levels. Diabetes Metab Syndr Obes. 2013;6:113-122. doi:10.2147/DMSO.S29222
Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33(12):e147-e167. doi:10.2337/dc10-9990
.Chen C, Zeng Y, Xu J, et al. Therapeutic effects of soluble dietary fiber consumption on type 2 diabetes mellitus. Exp Ther Med. 2016;12(2):1232-1242. doi:10.3892/etm.2016.3377
Vega-López S, Venn BJ, Slavin JL. Relevance of the Glycemic Index and Glycemic Load for Body Weight, Diabetes, and Cardiovascular Disease. Nutrients. 2018;10(10):1361. Published 2018 Sep 22. doi:10.3390/nu10101361
Bhupathiraju SN, Tobias DK, Malik VS, et al. Glycemic index, glycemic load, and risk of type 2 diabetes: results from 3 large US cohorts and an updated meta-analysis. Am J Clin Nutr. 2014;100(1):218-232. doi:10.3945/ajcn.113.079533
Vega-López S, Venn BJ, Slavin JL. Relevance of the Glycemic Index and Glycemic Load for Body Weight, Diabetes, and Cardiovascular Disease. Nutrients. 2018;10(10):1361. Published 2018 Sep 22. doi:10.3390/nu10101361
The InterAct consortium. Consumption of sweet beverages and type 2 diabetes incidence in European adults: results from EPIC-InterAct. Diabetologia 56, 1520–1530 (2013).